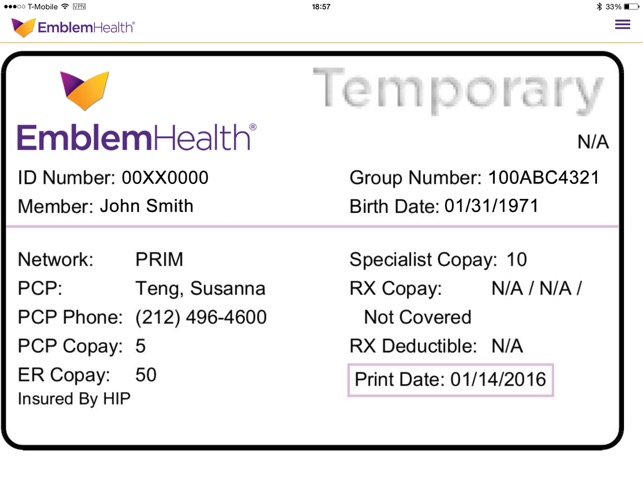
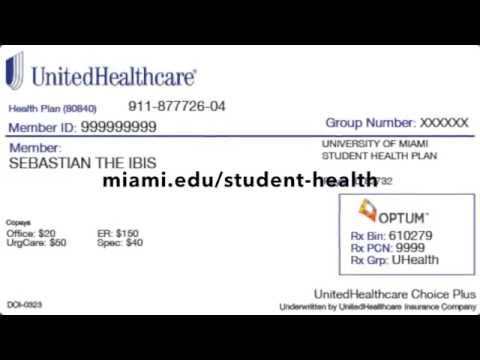
Each person covered by a health insurance plan has a unique ID number that allows healthcare providers and their staff to verify coverage and arrange payment for services. It's also the number health insurers use to look up specific members and answer questions about claims and benefits. If you're the policyholder, the last two digits in your number might be 00, while others on the policy might have numbers ending in 01, 02, etc. A member ID number and group number allow healthcare providers to verify your coverage and file insurance claims for health care services. It also helps UnitedHealthcare advocates answer questions about benefits and claims.
Your member ID number and group number allow healthcare providers to verify your coverage and file claims for health care services. These numbers also help UnitedHealthcare advocates answer questions about your benefits and claims. Your insurance company may provide out-of-area coverage through a different health care provider network.
If so, the name of that network will likely be on your insurance card. This is the network you'll want to seek out if you need access to healthcare while you're away on vacation, or out of town on a business trip. Many health insurance cards show the amount you will pay (your out-of-pocket costs) for common visits to your primary care physician , specialists, urgent care, and the emergency department.
If you see two numbers, the first is your cost when you see an in-network provider, and the second—usually higher—is your cost when you see an out-of-network provider. For example, when you're referred to a specific specialist or sent to a specific hospital, they may not be in your insurer's network. Your health insurance policy number is typically your member ID number.
This number is usually located on your health insurance card so it is easily accessible and your health care provider can use it to verify your coverage and eligibility. If you forget or aren't sure what type of health insurance plan you have , you can find out on your BCBS ID card. If you have an HMO, your card may also list the physician or group you've selected for primary care. Determining whether a provider is in-network is an important part of choosing a primary care physician. If you elected SHCA coverage, added dependents or changed your primary care physician during Open Enrollment, Aetna will send you a new member card by Jan. 1.
What Does Group Mean On Insurance Card All other current members can view the updated digital card sometime after Jan. 1. You can view and download your card from the Aetna Health mobile application, or via the Aetna.com website on your desktop. The back of your member ID card includes contact information for providers and pharmacists to submit claims.
It also includes the member website and health plan phone number, where you can check benefits, view claims, find a doctor, ask questions and more. The descriptions below apply to most private health insurance ID cards in the United States. If you live outside the U.S. or have government-provided insurance, you may see some different fields on your card. If you lose your health insurance card with your policy and group number on it, it is important to contact your health insurance company right away and let them know. Call your insurance provider's customer service number and a representative should be able to help you. If you have family members listed as dependents on your health insurance plan, they may each have their own unique policy number as it is used for identification purposes and billing procedures.
Your health insurance policy number is what identifies you as a covered individual under your current or previous plans. It's important because if you change jobs or get married, divorced, etc., then your HIPN will need to match the new situation. If you move out of state, your HIPN needs to reflect where you live now. In some cases your ID number will change, such as if you switch health insurance plans during open enrollment. But, your number should stay the same if your plan doesn't change. If you are unsure of whether your ID number has changed, call Customer Service at the number listed on your ID card.
It is assigned to your employer by the insurance company and can also be beneficial for both you and your health care provider in finding out what your coverage entails and submitting claims. If you have coverage from an employer-based health insurance plan, there will most likely be a group number on your insurance card, as well. The back of the member ID card includes the member website and phone numbers to connect with customer service, speak with a nurse and discuss behavioral health. It also includes contact information for providers and pharmacists to submit insurance claims.
The back of the member ID card may include phone numbers to connect with customer service, speak with a nurse and find behavioral health support. It also includes contact information for providers and pharmacists to submit claims. After going through, one can get a pretty straightforward idea about the health insurance cards. I think that it is a good idea to maintain an effective health insurance coverage.
I think that the cards should also link the patient's previous medical history. Different insurance plans sometimes cover different pharmacy networks. For example, CDPHP employer plans use a Premier network; CDPHP individual plans use a Value network; and CDPHP plans for seniors use the Medicare network. Your marketplace plan ID is different than your application ID.
You will receive your application ID along with your eligibility results after you apply for marketplace coverage. After you receive your application ID, you will need it to continue on with your application, compare different plans and prices, and to officially complete your health care enrollment. You can also provide this number to your health insurance company so they can look up your information when you have questions about your benefits and any recent claims. Keep it in a safe, easily accessible place like your wallet. Your card contains key information about your health insurance coverage that is required when you need care or pick up a prescription at the pharmacy. Keeping your card in a secure location will also help protect you from medical identity theft.
A simple, secure, and convenient way to manage your health care. In addition to access to a digital ID card, the App also provides you with the ability to find a doctor, review claims, and keep track of your medications. Our phones, keys, driver's licenses and credit cards are kept at our fingertips at all times. Those items are unique to each of us, and provide access to the things we need. When it comes to healthcare services, that item is your Blue Cross Blue Shield ID card.
All members, including dependents under 18, can access a digital ID card. These are available via our HAP OnTheGo mobile app or by logging in at hap.org. When taking children under 18 for services, parents should show their own card.
Most health insurance cards contain straightforward identification information about the people covered and the policy you have. Your member ID card – like the example shown here – identifies you as a CareFirst member and shows important information about you and your covered benefits. Each family member on your plan should have a card with their name on it. Make sure to always present your ID card when receiving services.
If you don't have your physical card, you can view it on your smartphone through My Account. To begin comparing health insurance providers rates, simply enter your ZIP Code above. The search engine will return a a wide range of health insurance companies who offer policies within your area.
This is a unique 14 digit identifier that may be a combination of both numbers and letters. When searching on the health care marketplace, you will be able to find a plan's ID number below the plan's name along with a preview of the plan's prices and coverage options. Your BCBS ID card has important contact information to help you reach your BCBS company.
Look on the back of your card to find the phone numbers for customer service and eligibility questions. You can also use our directory to find your BCBS company's website.There you can log into your account and find out more about how to contact the company that provides you service. Here are some examples of UnitedHealthcare member ID cards. Your member ID card may vary depending on your specific health plan and coverage. We encourage you to reach out to your health plan's member services department so that they may assist you with specific questions about your ID card and benefits. If your plan includes benefits for prescription drugs, you will also find some information related to them on your health insurance ID card.
Some insurance companies give specific names to certain plans, like those available through the healthcare exchange, instead of using group numbers . This is the name of your insurance company and one or more ways to reach them, like their website and phone numbers for customer service or other specific needs. Your member ID number identifies you as a covered member of Blue Cross and Blue Shield of Illinois. It's very important because it is how you access your benefits when you need care, much like a credit card lets you use your account to make purchases. Your member ID number connects you to your information in our systems, and is what providers use to make sure you are covered for a treatment or medicine when you seek care. Please present your insurance ID card whenever you fill a prescription and receive covered medical care.
Your BCBS ID card has your member number, and in some cases, your employer group number. Your member number, also known as your identification number, is listed directly below your name. You'll need this information when receiving medical services at the doctor or pharmacy, or when calling customer service for assistance. If your group number is available, you'll find it directly below your member number. It identifies you and lets your doctors and other providers know how to submit your claims.
UnitedHealthcare® members with plans through an employer may download the UnitedHealthcare app to view and show their member ID card on their smartphone or tablet. You may not think about your health insurance ID card very often. After all, it probably spends most of its time in your wallet—until you, your doctor, or another medical provider really need it. If you elected Kaiser or added dependents during Open Enrollment, Kaiser will send you a new member card before Jan. 1. Note that while Kaiser is still producing physical cards, they are moving away from cards with embossed lettering to cards that are flat and laminated. All members will be able to access their new cards digitally through the Kaiser mobile app by Jan. 1.
To view and download your card, log into the new EngagementPoint app (or create a new account if you haven't yet). Note that you can access EngagementPoint from your desktop or mobile device. In the navigation, "ID Cards" is listed at the top, under "Home."
If you've opted into electronic delivery of Blue Shield's communications, you won't receive an ID card by mail. New plan members can expect a new ID card in the mail by Jan. 1. All medical plan providers have made it easy for you to download and print your card digitally and important information is being added to your card for 2022.
If you have a suitcase on your member ID card, you can also find and receive certain levels of healthcare benefits when you live or travel across the country. Yourpolicy number on your health insurance cardwill not be the same as your group number. Thepolicy number on health insurancerefers to your individual member number, but the group number is different.
Network - This is the group of doctors and hospitals you can go to for care. To find a provider in your network, log in at hap.org and click on Find a Doctor/Facility and then click on Search for a Doctor or Facility. ID number - Identifies you as a HAP member and is the primary information providers use to get claims processed. It's also the number you'll use to register at your hap.org account. If you are the policyholder, your name will be on the card. If you have dependents—like a spouse or children—on your health insurance policy, their names might be listed on your card, too.
If you are not the policyholder, then your card may show your name and the policyholder's name in separate fields. At this time of year, employees often ask if they'll be getting a new card, or what happens if they need services or prescriptions before they have a new card in hand. It's important to take your member ID card with you when you seek care, so thatyour doctor'soffice has your insurance information. Without it, you may be billed wrongly for treatment or services. You will also need your ID number when you call Customer Service or pay your bill. My Blueprint is a members-only website that will help you understand and manage your health plan so you're able to find quality, patient-focused healthcare at the best possible price.
The Blue Cross Blue Shield System is made up of 35 independent and locally operated companies. To access your member services, please visit your BCBS company. If you need an additional card, log in to your hap.org account and request one to be mailed, or download one to use immediately.
If you have questions about your coverage, please call a Customer Service specialist at the number on your HAP ID card. Tiered access - If you have a tiered network, you might have different out-of-pocket costs for providers in the different tiers. When you log in at hap.org and search for a provider, if you have a tiered network, each provider will list which tier they are in.
Your card also has information about the type of plan you have and your provider network. Prescriptions are processed through a company that administers HAP's drug benefits. The Rx numbers on your card tell your pharmacy how to process your claim so your prescriptions get paid correctly. Unfortunately, new health care fraud and abuse schemes are constantly occurring. You can help protect yourself and your family by staying informed. Now that you're signed up, we'll send you deadline reminders, plus tips about how to get enrolled, stay enrolled, and get the most from your health insurance.
BlueAdvantage Administrators of Arkansas is an Independent Licensee of the Blue Cross and Blue Shield Association and is licensed to offer health plans in all 75 counties of Arkansas. A policy number is a unique identifying number given to every person enrolled with a specific health insurer. Our insurance industry partnerships don't influence our content. To compare quotes from many different insurance providers please enter your ZIP code above to use the free quote tool. You can use the first three numbers on your member ID card to find your local BCBS company's website. There, you can log into your account and access your benefits.